By Izzar Linares
Illustration by Ofure Itua
This article references the most reliable and up-to-date data.
INTRODUCTION
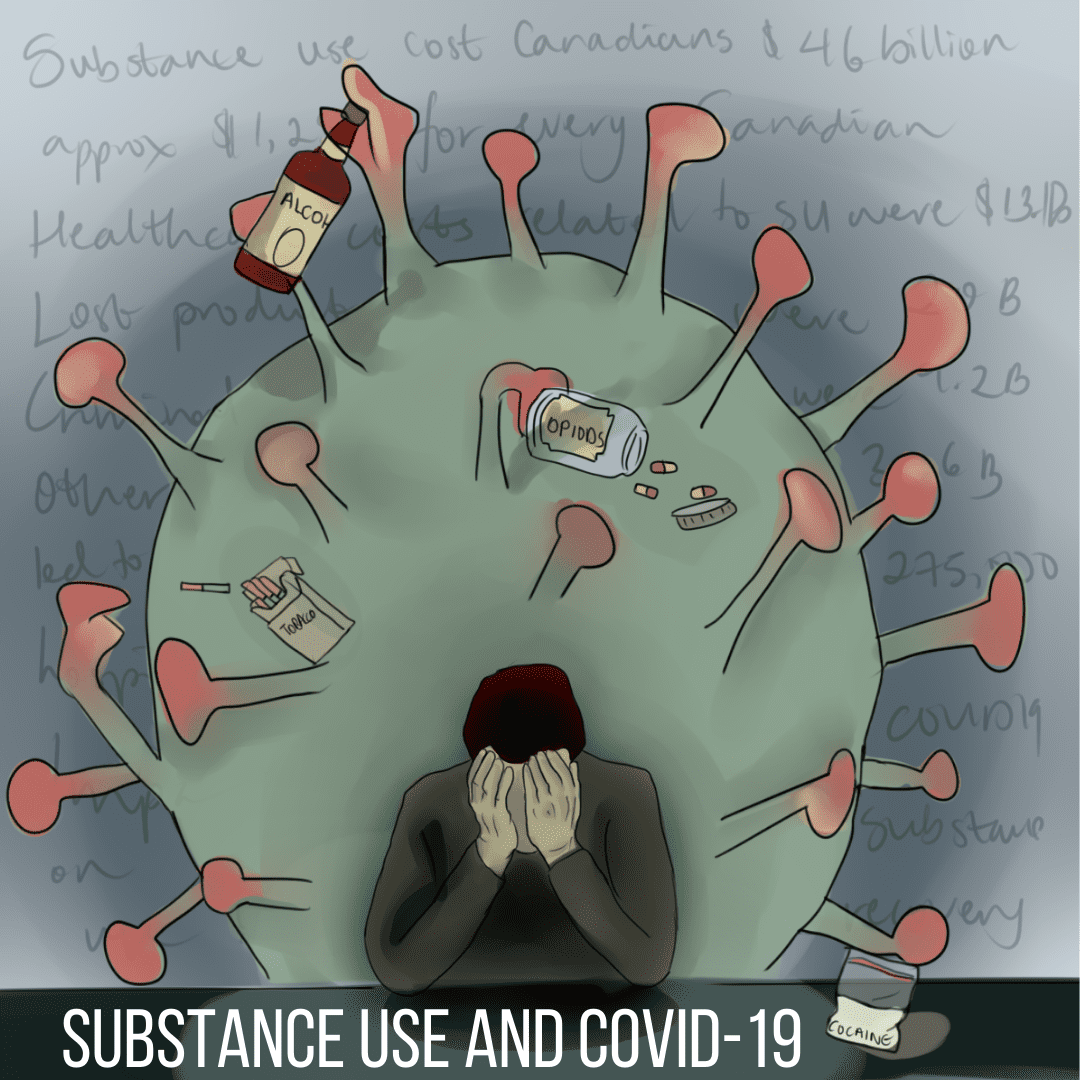
In 2017, substance use (SU) cost Canadians almost $46.0 billion, equaling approximately $1,258 for every Canadian regardless of age [1]:
- Healthcare costs related to SU were $13.1 billion (28.6% of the total cost of SU) or $386 per person in Canada
- Lost productivity costs related to SU were $20.0 billion (43.6% of the total cost of SU) or $548 per Canadian.
- Criminal justice costs associated with SU were $9.2 billion (20% of the total cost of SU) or $253 for every Canadian
- Other direct costs (costs across several categories like research and prevention, damage to motor vehicles, fire damage) contributed over $3.6 billion (7.8% of the total cost of SU) or $100 per Canadian.
In 2017, substance use led to over 275,000 hospitalizations and contributed to nearly 75,000 lives. The four substances associated with the most considerable costs were alcohol, tobacco, opioids, and cocaine [1].
In 2017, Canada was not in a historic pandemic, so while very little is known about how COVID-19 will impact Canadian substance use cost, past disasters (e.g. tornadoes, floods, hurricanes, etc.) tells us that use of substance generally increases following major traumatic events [2,3]. With the COVID-19 pandemic changing the lives of many across Canada, it presents even more unique challenges for people with substance use and addiction and in recovery. This article hopes to showcase recent research and spark a conversation on the impact of COVID-19 on substance use.
SUBSTANCE USE and COVID-19
Substance use affects more than just a Canadian’s health. It affects several areas, including healthcare, lost productivity and criminal justice. While very little is known about how COVID-19 will impact the Canadian substance use cost, we know substance use is rising in Canada, mainly alcohol, which is easier to measure and report. A recent study [4] showed that nearly nine in ten Canadians reported staying at home more due to COVID-19 and that one in five Canadians staying at home more reported that their alcohol consumption has increased since they have been staying at home more. The study [4] also stated that the top reported causes for increased alcohol consumption were boredom, stress, and lack of a regular schedule. As aforementioned, the COVID-19 pandemic presents exceptional challenges for people with substance use and addiction and in recovery. While the impact of COVID-19 on illegal drug use is also not yet fully known, COVID-19 could make current addicts more vulnerable to complications of substance use. For example, individuals who regularly use cigars, opioids, crack-cocaine, and vaporizers are already at risk of rhombic respiratory diseases and pulmonary complications/diseases, which puts them at a higher risk for severe complications of COVID-19 (due to the diminished lung capacity from COVID-19). Moreover, while social distancing, isolation or quarantine are essential measures to prevent the transmission of COVID-19, these conditions can be associated with emotions such as loneliness, irritability, anxiety, fear, sadness and anger, and it is these negative emotions that are known to trigger a relapse, even in those long-term abstainers, or intensify drug consumption [5]. Additionally, withdrawal occurring during mandatory lockdown could cause individuals to go outside for drugs, thus jeopardizing their health and preventive strategies [6]. Another risk of COVID-19 on those suffering from addictions is decreased access to health care [7]. Since the major medical efforts are geared towards the COVID-19 pandemic, medical assistance is limited, and thus access to health care further underserves individuals with addiction. Additionally, many 12-step programs have cancelled meetings. This means there is a good chance that people might relapse or intensify drug consumption as in-person meetings are often an essential part of the recovery process. Homelessness may also disrupt preventive strategies due to poor public health among the homeless (e.g. non-hygienic disposal of bodily waste, discarded syringes, cigarette butts, etc.) and individuals with addictions often sleep in crowded places during the night, thus making them potential vectors of transmission.
CONCLUSION
COVID-19 is a danger to the entire population; however, the impact of the coronavirus disease on those suffering from substance use and addiction is unique. Those who struggle with substance use are already a high-risk population and different risk factors associated with substance use are predicted to cause this population to be profoundly affected by this global pandemic.